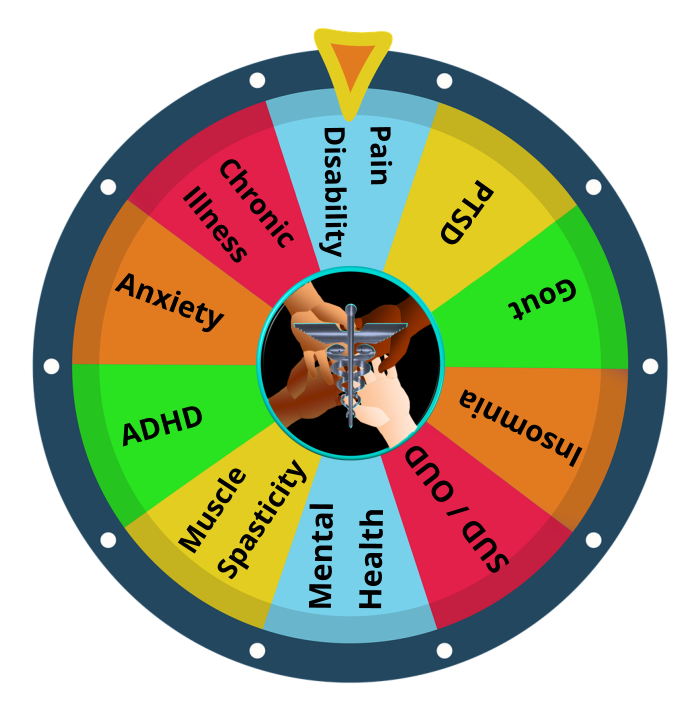
Patients Forced to Play Medical Roulette
For patients with rare disease, complex chronic illnesses and disabilities navigating the health care system has become a fight for survival. Patients experience systemic disability discrimination and bias when attempting to obtain or retain access to treatments and medications that are critical to maintaining their health.
Due to interference with the practice of medicine, patients are being forced to play a dangerous, potentially deadly game of medical roulette. It’s a game that patients don’t want to play, but there are no alternatives for those with multiple medical conditions who require controlled substances to manage their health. They are coerced into agreeing to discontinue a vital medication as a condition of retaining or obtaining treatment for a debilitating medical condition. In some cases, when a patient cannot discontinue a medication without severe adverse, potentially life threatening consequences, they are discharged from the medical practice.
Physician autonomy has been undermined by insurance companies, politicians, state medical boards, law enforcement, special interest groups, and non-medical administrators at healthcare facilities. Most, if not all use algorithms based on a subjective definition of legitimate medical treatment. Clinicians are being coerced and even paid more/incentivized to not prescribe controlled substances.
Medical professionals are caught in a catch-22 situation. If they provide patient-centered care or treat patients who live in a healthcare desert, they risk being targeted for investigation and prosecution. If they base treatment decisions on blanket policies, hoping to avoid unwarranted persecution for exercising their clinical judgment, they are violating the American’s with Disabilities Act.
Since the Centers for Disease Control issued Chronic Pain Guidelines for Primary Care Physicians (PCP) in 2016, my daughter’s life has been put in jeopardy repeatedly. She is a rare disease patient with multiple overlapping chronic illnesses that cause significant disability. The systemic discrimination she has faced when attempting to retain her treatment regimen for her disabilities has been profound.
She has experienced life-threatening, involuntary, rapid tapering and abrupt discontinuation of essential pain medication on multiple occasions despite her clinicians being fully aware that she has a heart condition and seizure disorder. One Pain Management (PM) specialist initiated a taper of 75% on day 1. His response when concerns were raised was “I know you need the medication. But, my practice is more important than your life. I’m too scared of the DEA to prescribe what you need.”
She’s been without a Pain Management specialist for over two years now. Her most recent PM discharged her from his practice when they adopted a new policy to not prescribe pain medication to anyone taking a benzodiazepine. Although her doctor was given medical documentation that discontinuation was not possible, he discharged her from the practice, rather than accommodating her disability and providing treatment based on her individual healthcare needs. We have been unable to locate any other PM willing to accept her as a patient due to her need to continue her current medication regimen to manage her seizure disorder.
She is now facing another dire threat to her health. Her insurance carrier recently purchased her primary care practice (PCP), and they have mandated she must be involuntarily tapered off her anti-seizure medication. All other classes of medicine have caused life-threatening adverse reactions. The PCP she’s seeing will be gone in less than two weeks. She’s now facing a situation where there are no reasonable choices. All outcomes are potentially life threatening:
- Attempting to live with an untreated seizure disorder and co-morbid heart condition;
- Rapid taper resulting in Benzodiazepine Withdrawal Syndrome, (a previous gap in treatment due to clinicians delay in sending in a refill resulted in a 10-day hospitalization);
- Taking a different class of medication known to cause life threatening adverse reaction, or
- Attempting to self-medicate via the illicit market.
Time is running out for her, and other patients in similar situations. There are no legal substitutions available to manage her seizure disorder. She’s facing an uncertain future where the risks of death due to medical neglect are high.
The climate of fear that is now controlling the practice of medicine must be eliminated to ensure that individuals with disabilities are able to obtain treatment based on their personal health care needs. Medical professionals must feel safe to act in the best interests of their patients, and not fear that doing so will result in unwarranted criminal investigations or charges. To help restore physician autonomy, ensure health equity, reduce discriminatory practices in medicine and improve the quality of life and function to disabled individuals, a petition has been issued requesting the following actions to correct this grievous inequity.
-
- The Department of Justice shall prepare and release guidance for “Pain, Policy Modification Requirements & the Americans with Disabilities Act.”
- The Department of Justice, all federal agencies and federally funded programs shall immediately cease any program that targets clinicians for investigation and/or prosecution that uses a subjective definition of Legitimate Medical Treatment.
- Congressional Hearings shall be scheduled by the House Oversight Committee and the Judiciary Committee to investigate these issues and form a plan for corrective action.


This same significant problem, the conflict of understanding palliative care, continues to arise and is negatively affecting many in the chronic illness community.
The true definition of palliative care is specialized medical care for people living with a serious illness. This should be universally recognized by all who participate in our healthcare system. (https://www.nia.nih.gov/health/what-are-palliative-care-and-hospice-care#:~:text=Palliative%20care%20is%20specialized%20medical,to%20cure%20their%20serious%20illness.).
I agree completely Tammy.
One of the most significant problems that patients who need palliative care encounter is that there’s a fundamental misconception that it’s exclusively for end of life care. Many states don’t have palliative definitions codified, so palliative care agencies set their own policies and definitions which can vary widely within the state and a city.
I hope and pray you can find help for your daughter. It is a horrible corrupt time in history that we have gov’t and insurance companies controlling the decisions of our doctors. In turn control the destiny of the patient which often times are under-treated or abandoned to suffer and die without pain relief. Cruel and inhumane.
Heartbreaking ?
Thank you Dora.
We had thought Palliative Care (PC) might potentially be the solution. But, in our area, the Palliative Care practices do not prescribe medication outside of Hospice. One PC company informed me that she didn’t meet *their* criteria, since she’s anticipated to live longer than 12 months. And, doesn’t have the *right* diagnosis. Although, she is profoundly disabled with multiple overlapping medical conditions that impair her ability to function, without a diagnosis of cancer, COPD or Congestive Heart Failure she doesn’t qualify.